New data suggest that margin marking prior to endoscopic mucosal resection (EMR) of large colorectal polyps reduces the risk of recurrence by 80% compared to traditional EMR.
A team of researchers led by Dennis Yang, MD, with the Center for Interventional Endoscopy at AdventHealth in Orlando, Florida, compared polyp recurrence after patients received a bordered EMR to recurrence after conventional EMR in a historical control group. They conclude that the simple margin marking strategy can offer an alternative to margin ablation.
Dr. Dennis Yang
The results of the study were published online in Gastrointestinal Endoscopy on November 29th.
A central, historical control study
A total of 210 patients (mean age 66 years; 56.2% women) with 210 polyps (mean size 30 mm; interquartile range: 25-40 mm) had either EMR with margin marking (EMR-MM; n = 74) or conventional EMR (n = 136 ). The groups had similar patient and lesion characteristics.
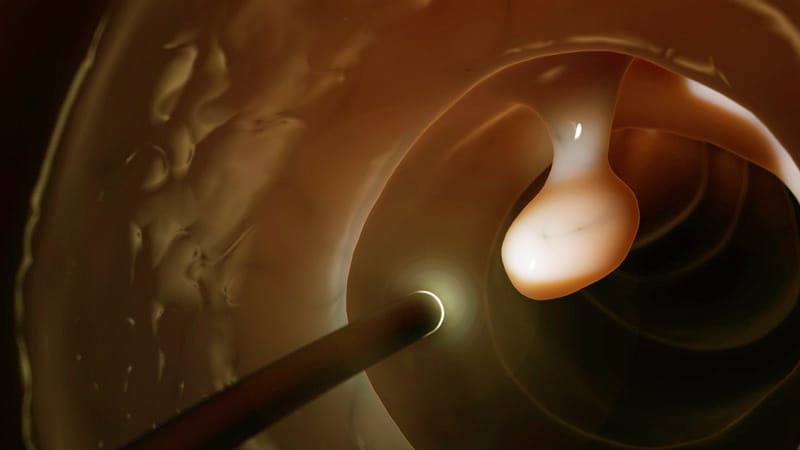
For EMR-MM, cautery marks were drawn along the lateral edges of the polyp with the tip of the loop. EMR followed with resection of the healthy mucosa with the markings.
Doctors can confirm a full resection, including a healthy margin, if no traces of cautery are visible after EMR, the authors write.
A control colonoscopy was performed after 3 to 6 months, the results of which were compared with historical controls.
After 6 months, EMR-MM resulted in a lower recurrence rate compared to the historical control group with traditional EMR (8% and 29%; P <0.001).
“This strategy allowed for a more reliable wide-field EMR, which may explain why our preliminary results showed an 80 percent reduction in the likelihood of recurrence even after controlling for other factors, including polyp size and histopathology,” the authors write.
The risk of recurrence was one of the main limitations of EMR compared to surgery, with rates ranging from 10 to 35%, the authors note, although it has fewer side effects and offers a better quality of life than surgery.
Yang told Medscape Medical News that several studies have looked at possible factors behind a recurrence that is believed to occur primarily on the lateral resection margins of the polyp.
“This is based on recent data that has shown that burning the resection margins after removing the lesion reduces recurrence,” he said. “Indirectly, this implies that with each resection we may think that we have the entire lesion on the lateral margins, but that is not the case.”
As Yang described, it was this implication that led to the premise of the study.
“If we were to make any visible markings outside the edges of the lesion, the markings would act as visual cues to let us know how much more tissue we needed for the resection, thereby helping us to have a more reliable method of ensuring clean resection margins . ”
Yang and colleagues also found that EMR-MM was not associated with an increase in side effects. In the multivariable analysis, EMR-MM was the main predictor of recurrence (odds ratio [OR], 0.20; 95% CI, 0.13-0.64; P = 0.003) apart from the polyp size (OR 2.81; 95% CI 1.35-6.01; P = 0.008).
Expert: Standard of care probably even better
Douglas Rex, MD, Distinguished Professor Emeritus of Medicine at Indiana University School of Medicine at Indianapolis, who was not involved in the study, told Medscape Medical News that he is not convinced that it is necessary or useful to Use the edge marking technique described in the paper on the current standard of care.

Dr. Douglas Rex
Rex explained that doctors are currently injecting large lesions submucosally with contrasting-colored fluid to delineate the edge of the polyp. This begs the question, if you can see the lesion well with this method, then do you need to place the markers before starting around the edge on the normal mucosa, as was the case with the edge marking group in this study?
Rex also noted that the researchers’ relapse rate in the control group is relatively high at 29%.
“Most of the evidence – if you look at the large meta-analyzes – suggests that the recurrence rate with traditional methods is around 15%,” he said.
He added that even the recurrence rate in the active treatment arm of the current study is much higher than the 2% -5% rate seen in recent thermal ablation studies by Klein and colleagues and Sidhu and colleagues, both published in Gastroenterology .
“The methods described in these two papers should be viewed as the current standard of care,” said Rex. “It’s not about either of them [margin-marking] Method.”
Yang agrees that the Klein and Sidhu studies are the standard of care, but says it is important to note that the 2% recurrence may not reflect actual practice by endoscopists of all skill levels.
“These are tightly controlled studies by very experienced endoscopists,” he said.
“Our data is not trying to replace what the high quality thermal ablation studies have shown. It’s about showing that this is a concept that could potentially help, ”he said.
“What I am proposing is a potential alternative that could be better. Of course we will not know until a comparative experiment is carried out. “
On this point, Yang and Rex agree.
Rex said a randomized controlled trial would clarify a few points and be useful in comparing the margin marking directly to the current standard of care, “which is to remove the whole thing and then burn the margin.”
“Based on what we’ve seen so far, I would say that the current standard of care has a very good chance of winning in terms of effectiveness as it’s hard to get below 2%. [recurrence]”He said.” And in terms of safety it could well win, because burning the margin is, at least in theory, safer than what you’re doing here. “
Rex said the edge marking can be beneficial in the form of EMR that does not involve submucosal injection: underwater EMR. There is no submucosal injection with underwater EMR, and some people will mark the edge in those cases, he said.
“I think it’s reasonable to do edge markings for underwater EMR,” said Rex.
Yang is a consultant for Boston Scientific, Olympus, Lumendi, and Steris. A co-author is a consultant to Olympus, Boston Scientific, Cook Medical, Merit, Microtech, Steris, Lumendi, and Fujifilm. Another co-author receives research grants from Steris and Cosmo / Aries Pharmaceuticals. Rex did not disclose any relevant financial relationships.
Gastrointestinal endoscopy. Published online November 29, 2021. https://www.giejournal.org/article/S0016-5107(21)01842-3/pdf
Marcia Frellick is a freelance journalist based in Chicago. She previously wrote for the Chicago Tribune, Science News, and Nurse.com, and was an editor for the Chicago Sun-Times, the Cincinnati Enquirer, and the St. Cloud (Minnesota) Times. Follow her on Twitter at @mfrellick.
For more news, follow Medscape on Facebook, Twitter, Instagram and YouTube.