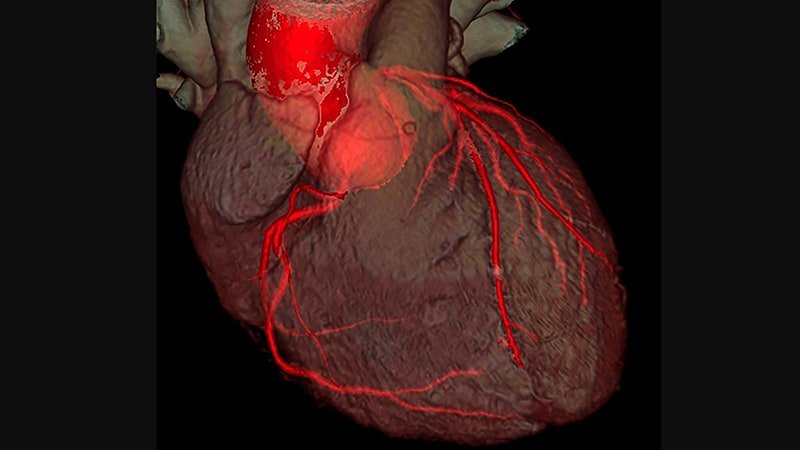
New research suggests that serial coronary CT angiography (CCTA) in patients with advanced coronary artery disease may provide new insights into the relationship between lipoprotein(a) and plaque progression over time.
Researchers examined data from 191 people with multivessel coronary artery disease who received prophylactic therapy with statins (95%) and antiplatelet agents (100%) in the single-centre Scottish DIAMOND study and compared baseline and 12-month CCTA compared to 160 patients were available.
As reported in the Journal of the American College of Cardiology, patients with high Lp(a), defined as at least 70 mg/dL, had higher high-density lipoprotein cholesterol and ASSIGN scores at baseline than patients with low Lp(a ), but had higher Lp(a) comparable coronary artery calcium (CAC) scores and total volume, calcified, noncalcified, and low attenuation plaque (LAP).
However, after 1 year, the LAP volume – a marker for necrotic core – increased by 26.2 mm3 in the high Lp(a) group and decreased by -0.7 mm3 in the low Lp(a) group (P = 0.020).
There was no significant difference in the change in total volume of calcified and non-calcified plaque volumes between groups.
In multivariate linear regression analysis adjusted for body mass index, ASSIGN score, and segment involvement score, LAP volume increased by 10.5% for each 50 mg/dL increment of Lp(a) (p = 0.034).
“It’s an exciting observation because we’ve done previous studies where we’ve shown the association of this particular type of plaque with future myocardial infarction,” senior author Marc R. Dweck, MD, PhD, University of Amsterdam, Netherlands, told theheart.org | Medscape Cardiology. “So you may have an explanation for the poor prognosis associated with high lipoprotein(a) levels and its association with cardiovascular events and myocardial infarction in particular.”
The team’s most recent SCOT-HEART analysis found that LAP load was a stronger predictor of myocardial infarction (MI) than cardiovascular risk scores, stenosis severity and CAC score, with MI risk almost five times greater, if the LAP was above 4%.
Questioning why the total calcified and uncalcified plaque volume did not change significantly with repeat CCTA in the present study, Dweck said it was possible that the sample was too small and the follow-up was too short, but also that “the overall Plaque volume really dominated by the fibrous plaque, which does not appear to be affected by Lp(a).” Nevertheless, the effect of Lp(a) on plaque with low attenuation was clearly present and was offset by the change in fibro-fatty plaque, the second most unstable plaque type, supported.
At 1 year, the fibro-fat-plaque volume was 55.0 mm3 in the high Lp(a) group versus -25.0 mm3 in the low Lp(a) group (p=0.020).
Lp(a) was associated with fibro-adipose plaque progression in univariate analysis (β = 6.7%; P = 0.034) and showed a trend in multivariate analysis (β = 6.0%; P = 0.062 ).
“This study shows that you can track changes in plaque over time and highlight important disease mechanisms and use them to understand the pathology of the disease,” said Dweck. “That encourages me a lot.”
What is new about the present study is that “it represents the beginning of our understanding of the role of Lp(a) in plaque progression,” Sotirios Tsimikas, MD, University of California San Diego, and Jagat Narula, MD, PhD, Icahn School of Medicine at Mount Sinai, New York, say in an accompanying commentary.
They note that previous studies, including the Dallas Heart Study, have had difficulty finding a strong association between Lp(a) and the extent or progression of CAC, although elevated Lp(a) and CAC identified higher-risk patients.
Similarly, a meta-analysis of intravascular ultrasound studies found an absolute difference of only 1.2% in atheroma volume in patients with elevated Lp(a), and a recent optical coherence tomography study found an association of Lp(a) with thin-capped fibroatheroma but not lipid core.
However, with only 36 patients with elevated Lp(a), the current results need to be validated in a larger data set, say Tsimikas and Narula.
Although Lp(a) is genetically elevated in about one in five people and measurement is recommended in the European dyslipidemia guidelines, testing rates are low, partly because it has been argued that there are no Lp(a)-lowering therapies, Dweck observed . This could change with the Phase 3 Lp(a)HORIZON cardiovascular outcomes study, which follows strong Phase 2 results with the antisense drug AKCEA-APO(a)-LRx and is enrolling patients similar to the current cohort.
“Ultimately, it comes down to this basic thing, that once you’ve done the test, you need action, and then insurers will happily pay for it and clinicians will ask for it. That’s why this study is so important,” Dweck said.
Tsimikas and Narula also point to the highly anticipated results of this study, which are expected in 2025. “A positive study is likely to lead to further studies and new drugs that could reinvigorate the use of imaging techniques that could also go beyond plaque volume and atherosclerosis to predict clinically relevant inflammation and atherothrombosis,” they conclude.
Dweck is supported by the British Heart Foundation and is a recipient of the 2015 Sir Jules Thorn Award for Biomedical Research; has received speaker honoraria from Pfizer and Novartis; and has received consulting fees from Novartis, Jupiter Bioventures and Silence Therapeutics. The disclosures of the co-authors are listed in the work. Tsimikas has dual appointments at the University of California San Diego (UCSD) and Ionis Pharmaceuticals; is a co-inventor and receives royalties from patents owned by UCSD; and is a co-founder and has an equity interest in Oxitope and its affiliated companies Kleanthi Diagnostics and Covicept Therapeutics. Narula states that she has no relevant financial relationships.
J Am Coll Cardiol. 2022;79:223-233, 234-237. Full text, editorial
Follow Patrice Wendling on Twitter: @pwendl. For more from theheart.org | Medscape Cardiology, join us on Twitter and Facebook.
For more updates, follow Medscape on Facebook, Twitter, Instagram, YouTube and LinkedIn.